Introduction
Although the phrase ‘chronic health condition’ seems to be a common one, when we break it down, what actually is it and how does it impact the lives of patients and those that care for them? This article will delve into the emotional, mental and socioeconomic burden of chronic disease and why we should all care about its impact.
Background
Chronic disease is characterised by an unpredictable illness journey, reduced physical capability, a change in appearance and/or a dependence on treatment and healthcare professionals. All of this ultimately creates a change in one’s life prospects and the lives of those caring for them. Approximately a quarter of the UK population suffers from a long-term health condition (Nuffield , 2024), whilst the Global Burden of Disease includes chronic diseases as one of the top five causes of death worldwide, responsible for between 10-20% of deaths respectively (Tinetti et al., 2012),
However, beyond the obvious physical risks associated with chronic disease, there is a less obvious mental burden. Research shows that people with long-term health conditions are 2-3 times more likely to develop a mental health condition than average. While over half of carers are also treated for anxiety, depression or stress.
At Smile, we recognise this association between physical illness and mental health challenges. For example, depression has been shown to worsen the risk of ischaemic disease, whilst being associated with increased morbidity and mortality (Wei, 1994). Additionally, persons’ with chronic health problems who have associated psychological conditions have a reduced adherence to treatment for their chronic health issues as is their ability to cope with pain associated with their disease (Kimmel, Peterson and Weihs, 1995).
Therefore at Smile, in order to support a person holistically to take account of their wellbeing as well as their physical condition, we incorporate the biopsychosocial model.
The Biopsychosocial Model
When looking at the impact of chronic disease, we should look at it from a biopsychosocial perspective. This model addresses disease through analysing three groups; biological, psychological and social. Biological are the factors associated with the physical symptoms of disease, psychological are the mental impacts of the disease and social encompasses interpersonal and community relationships which are affected by the condition.
Through evaluating the impact of all three, one can have a holistic view of the disease and address each of these factors for the betterment of the patient (Megan, 2021). Already this model is employed on a wide scale. For example, the treatment of irritable bowel syndrome includes antidepressant and anti-anxiety pharmacology and psychotherapy which involves CBT and hypnotherapy (Tanaka et al., 2011).
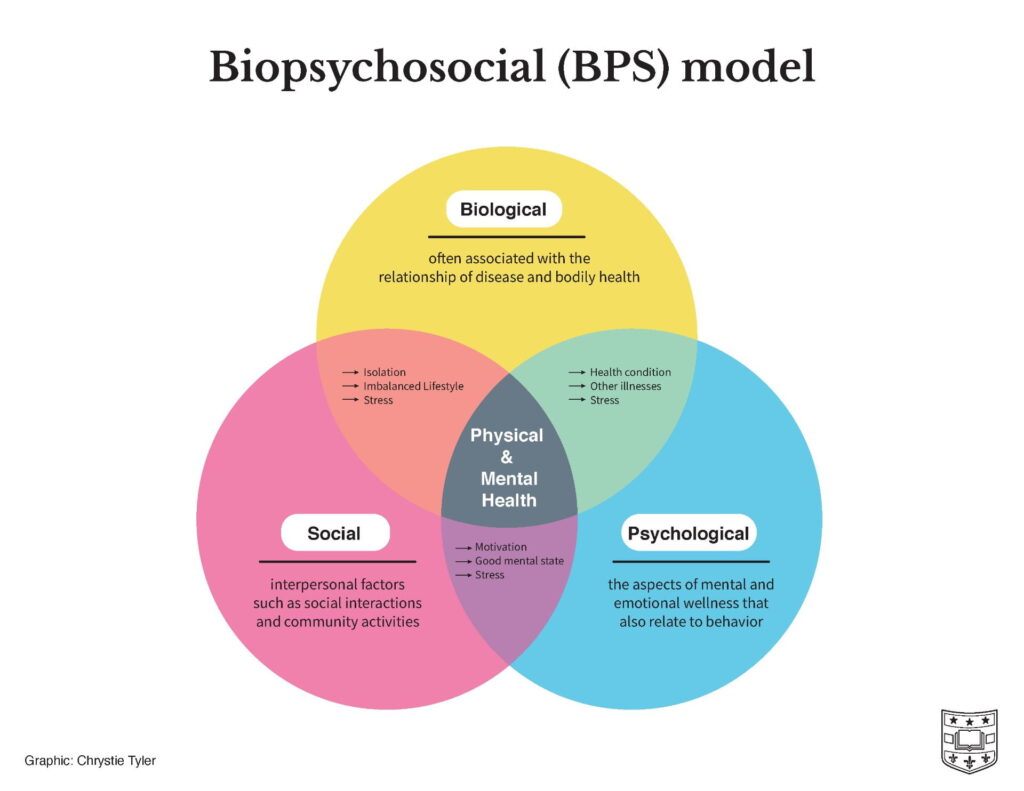
Illustration of the Biopsychosocial model (Megal, 2021)
At Smile, we go one step even further by also recognising the impact of disease on caregivers. Studies have found that unprepared informal caregivers suffer in particular, as they are forced to quickly cope with various competing stressors ranging from their own jobs and duties to a loss of their own identity and the responsibilities of another person (Janson et al., 2022).
Chronic health conditions and pain
Chronic health conditions have been found by numerous studies to be associated with long term pain (Ma et al., 2021). Patients who are constantly in pain are more likely to develop muscle soreness (Pope et al., 2015), leading to potential irritability and a restless sleep pattern, contributing to anxiety or depression (Amtmann et al., 2015). More severe pain has been associated with higher rates of depression, and those with chronic conditions are twice as likely to be depressed as those without ones (Read et al., 2017), due to the long-term nature of the disease and its impact on quality of life, affecting physical, social, emotional and financial health (Ma et al., 2021). This creates a vicious cycle where depression, disease and pain are all interlinked, warranting consideration of all factors when creating a treatment plan.
Chronic health conditions and the impact of them on ones’ wider life
To not address the impacts of chronic health conditions upon the patients’ wider life, ranging from job stressors to the impact upon their self worth would be neglecting a huge part of the condition. Without being able to fulfil their usual social roles, this leads some to have a much lower self-worth and sense of powerlessness about their own life, contributing to a lower mood and potentially depressive symptoms (Santos et al., 2017).
Beyond this, the stresses of meeting performance expectations at work whilst dealing with a chronic condition creates an additional mental and physical strain for people with chronic illnesses. People may have to take time off for doctors appointments or not be able to work to their full ability due to fatigue or mental health concerns. As Catherine Hale, the Director of Chronic Illness Inclusion describes ‘as a result, employees often feel obliged to work even when they should be resting, which has a detrimental impact on their health and wellbeing (How chronic illness shapes body image and identity 2023).’
Feeding into the idea of those with chronic conditions having a lower self worth are studies demonstrating that as a result of their physical symptoms, negative body images and self-perception may arise. Especially if this occurs during childhood, it can be a critical factor in their long-lasting mental health and potential social isolation. For example, a Psychology Today interview from a child with chronic disease explained ‘in high school, I would hide my body with pullovers because I knew it could not be trusted…it was easier to stay away from others (How chronic illness shapes body image and identity 2023).’
How do chronic health issues affect caregivers?
Although caring for a loved one can be extremely fulfilling as it draws the caregiver and receiver closer together, it may also become overwhelming, emotionally challenging and socially isolating. Many caregivers therefore have unmet psychological needs due to the significant demand of their new duties to fulfil. Approaching their needs within the biopsychosocial framework highlights the impact upon the caregivers’ wider life encompassing their social, physical, emotional and financial health.
Research says that one of the most common impacts on caregivers is a change in the dynamic between the relationship with the family member who is receiving care (Sullivan & Miller, 2015). It can become more task-focussed, whilst relationships with their other family members and friends may become more restrained as the caregiving requires more energy and time.
As an interview with a caregiver for Mind explained, even when they are invited to social plans, unless alternative care is available ‘I have to cancel what I wanted to do.’ Some caregivers describe this contributing to a ‘loss of identity’, as they no longer have the time nor energy to engage in hobbies and social engagements which previously formed part of their identity. At Smile, we focus on creating a community so that caregivers as well as those with chronic conditions may access the support and camaraderie they need.
This loss of identity can contribute to the emotional impact of being a family caregiver. As the caregiver has less time to engage in more positive coping strategies such as hobbies and social engagements, their negative emotions can become overwhelming. Such emotions may range from anger at their situation, to guilt at feeling like this, or nostalgia for the loss of the life they had hoped for. The stress of caregiving can even contribute to psychological disorders such as anxiety and depression (How chronic illness shapes body image and identity 2023), however few seek the needed help, perhaps due to a feeling that they do not have the time to do so, or that they are so tired of visiting doctors with their partner that the idea of going again is off-putting.
Not all caregivers are affected equally
In lower socioeconomic families, where the primary caregiver is also the primary wage earner, it adds even more stress to the caregiver. Here, any potential reduced performance at work may have huge financial consequences for their own and their family’s lifestyle, inevitably worsening their wellbeing. This stress is compounded when we consider that children from socioeconomic underprivileged families are twice as likely to experience chronic illness such as asthma, obesity and mental illness, compared to those of wealthier backgrounds (Ruijsbroek et al., 2011).
Studies have shown that especially when a child has a chronic condition, often the mother plays the main role of caregiving, in addition to domestic work and other parenting responsibilities (León-Campos et al., 2023). Caring for children is a demanding undertaking which affects the caregiver’s wellbeing in a multitude of ways.
Conclusion
As we can see, the word ‘chronic health conditions’ really only alludes to the obvious physical symptoms and neglects to describe the much wider picture of emotional, psychological, financial stresses which both patients and their caregivers experience. Such stressors can also alter the caregiver- receiver dynamic, and their relationship with others in their social circle, leading to an increased psychological burden.
Although this paints a bleak picture, it is important to remember you are not alone. Our goal at Smile is to help as many people as possible live well alongside a long-term health condition, and through our trained and experienced therapists, apps and workshops, we aim to support all aspects of your care holistically, whilst building a community that can appreciate what you are going through.
Amtmann, D. et al. (2015b) ‘Pain affects depression through anxiety, fatigue, and sleep in multiple sclerosis.’, Rehabilitation Psychology, 60(1), pp. 81–90. doi:10.1037/rep0000027.
Care and support for long term conditions (no date) Nuffield Trust. Available at: https://www.nuffieldtrust.org.uk/resource/care-and-support-for-long-term-conditions#:~:text=In%20England%2C%20more%20than%2015,with%20medication%20or%20other%20therapies (Accessed: 19 August 2024).
How chronic illness shapes body image and identity (no date) Psychology Today. Available at: https://www.psychologytoday.com/gb/blog/your-brain-on-body-dysmorphia/202301/how-chronic-illness-shapes-body-image-and-identity#:~:text=Studies%20find%20that%20chronic%20illness,with%20a%20negative%20body%20image.&text=While%20this%20is%20perhaps%20not,including%20eating%20disorders%20and%20depression (Accessed: 19 August 2024).
León-Campos, Á. et al. (2023) ‘Quality of life, physical and mental health, and economic evaluation of family caregivers of chronic dependent children: INFAPRINT cohort study protocol’, International Journal of Environmental Research and Public Health, 20(6), p. 5081. doi:10.3390/ijerph20065081.
Janson, P. et al. (2022) ‘Mortality, morbidity and health-related outcomes in informal caregivers compared to non-caregivers: A systematic review’, International Journal of Environmental Research and Public Health, 19(10), p. 5864. doi:10.3390/ijerph19105864.
Ma, Y. et al. (2021) ‘Relationship between chronic diseases and depression: The mediating effect of pain’, BMC Psychiatry, 21(1). doi:10.1186/s12888-021-03428-3.
Megan (2021) Three aspects of health and healing: The biopsychosocial model in medicine, Department of Surgery. Available at: https://surgery.wustl.edu/three-aspects-of-health-and-healing-the-biopsychosocial-model/ (Accessed: 19 August 2024).
Nuffield (2024) Care and support for long term conditions, Nuffield Trust. Available at: https://www.nuffieldtrust.org.uk/resource/care-and-support-for-long-term-conditions#:~:text=In
Smile is a mental health app for people managing chronic physical health conditions. To access the resources mentioned above, download the app now from Google Play or Apple App store.